Intractable migraine (also know as status migrainosus) is a persistent or chronic, debilitating migraine without aura that significantly affects a person’s ability to function. Even when affected individuals take steps to control triggers and make deliberate lifestyle changes, it still has a major impact on their quality of life.
They typically do not respond to the most common preventative medications (medication taken daily to decrease headache frequency), such as beta-blockers, tricyclics, anticonvulsants, and calcium channel blockers.
These migraines do not usually respond to abortive medications (acute medication taken at head onset) either. Triptans, a class of prescription medications that induce vasoconstriction, and nonsteroidal anti-inflammatory drugs usually fail as well. The trials to find a treatment that actually brings relief are usually quite long and arduous. All too often relief is never found.
Also known as refractory migraines, they are often described as “relentless” and “never ending.” It is a fact of life for so many people. They go to bed with it, wake up with it, and struggle to function through the day despite the discomfort, nausea, vertigo, and visual disturbances that often accompany these incapacitating migraines. They can be dangerous and should be taken seriously – treated as a medical emergency.
Axon optics caught up with Dr. Jonathan Cabin of The Migraine Institute in Beverly Hills, California to get some insight into intractable migraine.
“Intractable migraine, also called Status Migrainosus, is a migraine that lasts over 72 hours and is notoriously difficult to relieve with standard migraine treatments,” says Dr. Cabin. “Normal migraines last four to 72 hours. Anything longer technically becomes an “intractable migraine”.
This intractable migraine guide is intended to provide patients with information about their condition as well as provide guidance on potential treatments that could bring much needed relief. The chronic nature of these migraines can wear on a person both physically and mentally. It is our hope that this guide will arm readers with information to alleviate their suffering.
Page Contents hide>
- 1 Signs and Symptoms of Intractable Migraine
- 2 Causes of Intractable Migraine
- 3 Diagnosing Intractable Migraine
- 4 Treatment for Intractable Migraine
- 5 Combating the Psychological Effects of Intractable Migraine
- 6 When to see a Doctor about Intractable Migraine
- 7 Talking to Your Doctor about Intractable Migraines
- 8 The Future of Treatment for Intractable Migraine
- 9 Resources for Intractable Migraine Patients
- 10 Resources
Signs and Symptoms of Intractable Migraine
The symptoms of intractable migraine are nearly identical to those of other types of migraines. Most patients experience these symptoms:
- Constant headache which involves the neck that lasts 72 hours or longer
- Visual disturbances such as flashing or sparkling lights
- Nausea
- Vomiting
- Tingling Sensation
- Light sensitivity
- Sound sensitivity
- Speech disturbances
- Dizziness
- Difficulty focusing or inability to think clearly
Since this migraine lasts for three days or longer, there are other potential complications that can arise. The symptoms above can lead to other conditions including:
- Sleep deprivation or sleep loss
- Dehydration
- Fatigue
- Hypoglycemia

Causes of Intractable Migraine
Intractable migraines are triggered by many of the same things that trigger regular migraines. While doctors don’t completely understand what causes migraines, they can agree that several key components play a significant role as migraine triggers: genetics, lifestyle, environment, and body chemistry.
They believe that when there is an upset or imbalance in any of these components, it causes changes within the brain stem which impact how it interacts with the trigeminal nerve. The trigeminal nerve is the largest of the cranial nerves and is comprised of three nerve branches: the maxillary nerve, the ophthalmic nerve, and the mandibular nerve.
The maxillary nerve and ophthalmic nerve are sensory nerves in the face and head while the mandibular nerve does double duty managing sensory functions as well as supplying motor function like biting and chewing. The largely sensory aspect of this nerve gives it the potential to be a substantial pathway for discomfort.
When a migraine trigger affects the trigeminal nerve, it transmits the sensations in the face and head. The result is migraine.
Common migraine triggers include:
- Genetics – a parent or family members suffers from migraines
- Hormonal changes (women) – seems to coincide with fluctuations in estrogen which can include premenstrual, menstrual, pregnancy, and menopause
- Stress – can be a migraine trigger as the body’s response to stress, or other stress-related issues, such as muscle tension, can create conditions that become in themselves migraine triggers
- Foods – processed foods, salty foods, high sugar foods, ad aged cheeses
- Food additives – monosodium glutamate (MSG), aspartame, nitrates
- Beverages – high caffeine drinks like coffee, tea, and sodas as well as alcohol – especially wine
- Fluctuations in wake-sleep patterns – getting too much sleep, jet lag, sleep deprivation, poor quality sleep
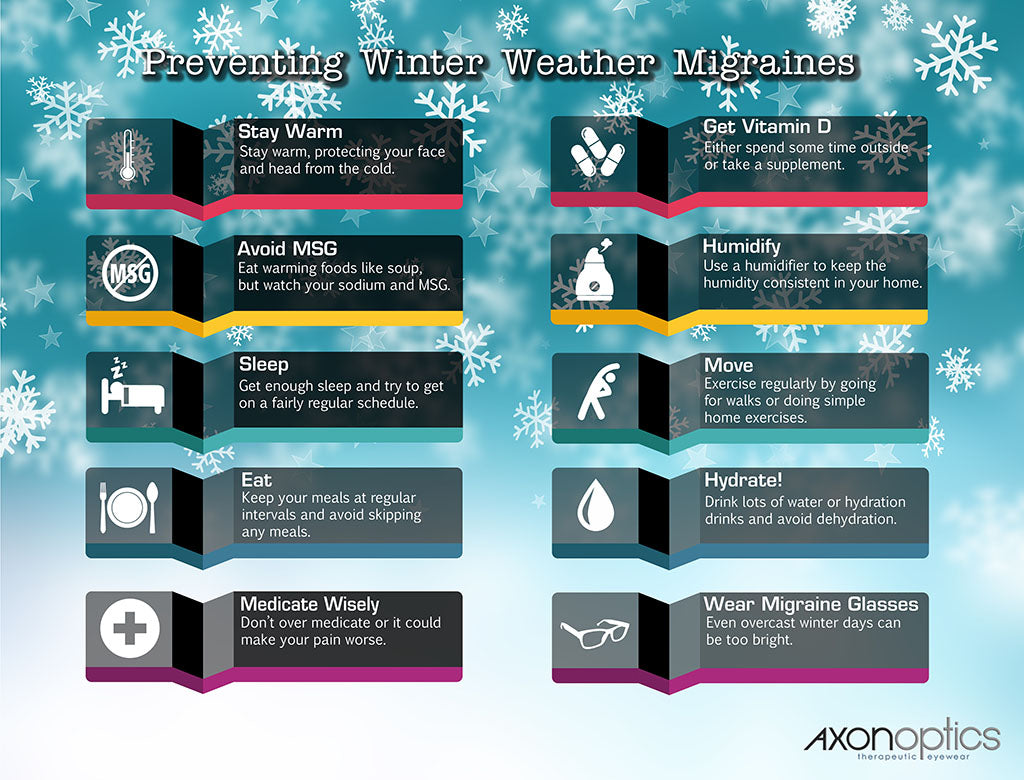
- Environmental changes – weather changes, change in barometric pressure, cold weather
- Sensory stimuli – bright lights and glare, strong smells, loud sounds, cold, heat
- Physical influences – intense exercise or physical exertion, straining, sexual activity
- Medications – nitroglycerin and other vasodilators, oral contraceptives, appetite suppressants (especially those with a stimulant like caffeine or other chemicals)
Age and gender also seem to often play a role in migraines. Women are three times more likely to get migraines after puberty. However, in childhood (pre-puberty), boys are affected more often than girls. Age also seems to play a part in a person’s propensity to get migraines as well as their frequency and intensity. Anyone at any age can get a migraine, but most people get their first migraine during adolescence. They tend to get progressively worse as the person ages, hitting a peak at some point during their 30s, then gradually declining in frequency and severity after that.
There is also a great deal of medical evidence that indicates an intractable migraine can be triggered or exacerbated by medication overuse. These rebound headaches occur when the patient overuses migraine medications, particularly NSAIDS like ibuprofen.
High doses of migraine medications can trigger the headaches, as can taking the medication (over-the-counter or prescription) for more than ten days within a month for three consecutive months.

Diagnosing Intractable Migraine
The diagnostic criteria for intractable migraine is similar to that of regular migraines. Doctors look for the common migraine symptoms such as the classic head pounding, nausea, vomiting, and visual disturbances. However, they also look for the distinct markers for status migrainosus, such as:
- Severity – intense or debilitating symptoms
- Duration – symptoms are unremitting and last 72 hours or more
The doctor will take a detailed history from the patient as well as conduct a physical examination. Tests such as neuroimaging may be run to rule out other health conditions or illnesses that could be causing the migraine.
Diagnosing intractable migraines is usually not a quick process. It often takes time as patient and doctor work together to identify patterns in migraine attacks. During the diagnostic process, it is vital that the patient maintain a detailed and complete headache diary. This will aid in not only finding patterns, but also in identifying triggers as well as treatments that provide relief.
All too often, patients give up because they feel that the diagnostic process is too long. They get tired, burned out, and lose hope. But only way that an effective treatment can be found is for the patient to persist in finding it. Keeping detailed notes and maintaining a good doctor-patient relationship will go a long way in finding a treatment that works.
Treatment for Intractable Migraine
Intractable migraines usually do not respond - or respond well - to most typical migraine treatments. While not all medications for migraines are effective in treating intractable migraine, there are some that seem to work. Several medication therapies have been identified that may halt intractable migraine (it should be noted that doctors advise patients who have blood vessel problems to avoid these medications):
- Dihydroergotamine (Migranal, DHE-45) – taken as a shot or nasal spray and can also be administered intravenously in the inpatient setting as part of a protocol known as the Raskin protocol
- Sumatriptan (Imitrex, Sumavel DosePro, Alsuma, Zecuity, and Onzetra) – available as a skin patch, nasal spray, shot, or pill
Prednisolone and corticosteroids dexamethasone (Dexpak, Dexamethasone Intensol) have been found to be effective for some patients.
Some patients find success with certain migraine preventative medications. While they may not prevent migraines entirely, they could decrease the number of attacks, especially those that turn into intractable migraines. These medications include:
- Beta blockers (commonly used to lower blood pressure) – nadolol (Corgard), atenolol (Tenormin), propranolol (Inderal, Hemangeol, InnoPran), and metoprolol (Toprol, Lopressor)
- Calcium channel blockers (also used for blood pressure), such as verapamil
- Tricyclics (a type of antidepressant) – Amitriptyline
- SNRIs (also an antidepressant) – Venlafaxine
- Anti-seizure medications – topiramate and valproate
- Botox
Other migraine medications may be effective, depending on the person. Some natural migraine remedies may also help.
Other treatments and preventative measures include:
Neruomodulation – Several neuromodulation techniques are proving to be very effective for intractable migraine. These include single pulse transcranial magnetic stimulation (sTMS), vagus nerve stimulation (VNS), supraorbital stimulation, or external trigeminal nerve stimulation (e-TNS), and occipital nerve stimulation (ONS). These have been shown to be safe and have very minimal side effects.
SphenoCath Procedure – Also called Sphenopalatine Ganglion Electrical Stimulation, this procedure involves administering Lidocaine through the nasal cavity to the Sphenopalatine Ganglion (SPG) nerve bundle. The lidocaine blocks the uncomfortable signals coming from the SPG nerve bundle and the migraine is eliminated.
Intravenous Propofol – This anesthetic causes sleepiness and relaxation, but has had great success as a treatment for intractable migraines. In one study, 63 of 77 participants who had intractable migraine reported that their migraines were completely gone.
Ketamine – This general anesthetic is commonly used to treat depression. However, a study published in Regional Anesthesia & Pain Medicine in November 2018, found that of the 61 participants, over 75 percent reported improvement in the intensity of their migraine after a five day inpatient treatment course.
Triptan – Daily use of this medication can help relieve some patients’ migraines.
Occipital Nerve Stimulation – This treatment involves stimulating the nerves in the back of the head, base of the skull, using electricity. It is intended to cause a tingling sensation which would mask the headache.
Chiropractic – Chiropractic care for migraines is a very effective treatment for some patients. Several studies show that chiropractic treatment, including the utilization of the Gonstead method, may help relieve and even help prevent migraine attacks, including intractable migraine.
Treatment may also include strategies to combat the symptoms as well. Medication for nausea and fluids for dehydration may also be administered IV or orally. It is important to get the body back into balance since that will help with the patient’s overall health as well as their body’s perception of their discomfort.
Precision tinted lenses like the patented Avulux® Migraine and Light Sensitivity Lens have been steadily growing in popularity. Many migraineurs credit them with helping their light sensitivity and migraine. Often referred to as “migraine glasses” by those who wear them, the effectiveness of the glasses is backed by studies as well as many very satisfied users.
The Avulux lens works by absorbing up to 97% of the most harmful blue, amber, and red light while allowing more than 70% green light (shown to be soothing) through.

Combating the Psychological Effects of Intractable Migraine
Psychiatric symptoms often accompany conditions that are debilitating and cause severe, persistent impact on daily life. Because intractable migraine disability tends to be unremitting, sometimes lasting for days, migraineurs often experience psychological effects such as depression and anxiety due to the relentless symptoms and disruption of their daily activities and quality of life.
Dr. Cabin weighed in on this phenomenon, “In terms of other psychological side effects during and after an intractable migraine, I always recommend the practice of mindfulness meditation, along with other stress reducing activities like yoga and acupuncture.” He continues, “Migraine is very real, but psychological distress can trigger migraines and make them feel much, much worse. Learning to manage this stress naturally is incredibly helpful for all migraine patients.”
Some doctors prescribe antidepressants or anti-anxiety medications to combat the psychological effects of intractable migraine. However, many doctors opt for more natural approaches, including regular exercise, no skipping meals, mood boosting supplements, exposure to sunlight, and a healthy, high protein diet that includes fresh produce, whole grains, and lean meats. This has the potential to not only ward off the anxiety and depression; it could even help with the migraine itself.
Yoga, herbs, and essential oils are also favorites of migraineurs because they often help with the anxiety and depression as well as with the migraines and associated symptoms. It is a process, though, to find what works. Different people respond to different substances and treatments, so it may take a little trial and error before finding something that effectively treats the psychological side of migraines. But treating this aspect of the condition is essential on so many levels.
When to See a Doctor About Intractable Migraine
Intractable migraines have the potential to become emergency situations. The longer they continue, the more serious they can become. A headache that lasts more than 72 hours certainly warrants medical attention, whether it is contacting one’s headache specialist or going to the emergency room.
“If experiencing a migraine for over 72 hours, it is important to get emergency medical attention,” says Dr. Cabin. “The symptoms of migraines – especially nausea and vomiting – can lead to dangerous and sometimes life-threatening conditions if they persist for over 72 hours. The emergency room can provide IV medications and fluid restoration, which is critical during this time period. “
When seeking emergency treatment for an intractable migraine, the patient should bring these items with them to ensure more appropriate, focused care:
- A statement from the diagnosing doctor or headache specialist that explains the migraine diagnosis, along with their name and contact information
- A history of their migraine, including treatments, medication trials, what treatment has worked and what has not, as well as any typical symptoms
- A complete list of medications with dosage information
- Migraine diary
- A friend for support and to act as an advocate. Ideally, this person is familiar with the patient’s migraines, symptoms, and triggers.
When a headache lasts longer than 72 hours, it is not a good idea to wait and see what happens. Research has already established links between migraines and a potentially increased risk for stroke and heart attack in women. There is also the possibility that the migraine is caused by an underlying condition.
Talking to Your Doctor About Intractable Migraines
Talking to your doctor about anything is rarely a pleasant experience, but talking about migraines can be even more difficult. There is a certain stigma attached to migraines that exists in the medical community and some doctors do not take the condition seriously. While headache specialists, neurologists, and some general practitioners do understand that migraines are more than just a headache, it isn’t always easy to find a healthcare provider who has that depth of understanding.
In any healthcare setting, be it a headache specialist, nurse practitioner, family doctor, or emergency department, these best practices for talking to your doctor about your intractable migraine can help focus care and expedite treatment:
- Be honest about intensity, frequency of migraines, lifestyle choices, behaviors, and symptoms – even if it is uncomfortable or embarrassing
- Always keep a detailed migraine diary
- When given medication, ask about dosage, side effects, expected outcome
- Write down any questions beforehand so they won’t be forgotten
- Know your family history
- Don’t be afraid to question something you don’t understand or that concerns you
Dr. Cabin offers this advice. “As I mentioned, if a patient is experiencing an intractable migraine, emergency medical attention is required. Once this migraine has subsided, it’s important to talk to your doctor about a lifestyle and medication regimen that can help control migraine headaches, and hopefully prevent intractable migraine from happening again.”
He continues, “In addition, many patients should consider interventional treatments – like minimally-invasive trigger point surgery and Botox – which can reduce the frequency, duration and intensity of migraines, including intractable migraines, without the typically harsh side effects of medications. Although few patients know about these treatments, they have been around for many years and are incredibly effective.”

The Future of Treatment for Intractable Migraine
Researchers all over the world are working diligently to find better ways to manage migraines, especially the debilitating intractable migraines. Each year brings more advances and a better understanding of this difficult disorder. We still have a long way to go, but progress is most definitely being made. Each new study brings us closer to a cure – and if not a cure, then at least relief.
Dr. Cabin had this to say, “As far as cutting-edge therapy for intractable migraines, the real work is being done in prevention. On the pharmacological side, exciting new medications have become available that significantly reduce migraine intensity and frequency with the use of antibody therapies, which marks a relatively new frontier for migraine treatment. On the surgical/interventional side, the latest minimally-invasive interventions can significantly and permanently reduce the frequency, duration and intensity of migraines in over 90% of chronic migraine sufferers.”
Resources for Intractable Migraine Patients
Intractable migraines usually evolve from regular migraines, although it is not unheard-of for a patient to begin their migraine journey experiencing them. However, the same way it typically takes time for a person’s migraines to become intractable (often months or sometimes even years), it usually is a process to return to normal and be migraine free. Very seldom will a new pill or treatment be the magic solution that takes it all away. Because of this long and often difficult process, emotional support is absolutely vital.
Having people who understand your condition and support you is one of the most effective coping mechanisms migraineurs can have. These websites offer support and help to people who have migraines and intractable migraines.
- MedHelp.org – Migraines & Headaches Community
- Status Migrainosus Facebook Group
- Patients Like Me – Status Migrainosus
- Alliance for Headache Disorders Advocacy (AHDA)
- Speak Your Migraine
Intractable migraines, as well as other types of migraines, are often a chronic illness. It is easy to withdraw from others, as your condition can make it difficult to be social or even maintain relationships. You may not want to “burden” others, or you may simply not have the energy to foster a relationship. Whatever the case, getting support in any capacity is helpful. The resources listed here will connect you to other people who have intractable migraine – just like you. They also offer valuable information and, most of all, hope for a future with fewer migraines.
Resources
Jonathan Cabin, MD
The Migraine Institute
9401 Wilshire Boulevard Suite 650
Beverly Hills, California 90212
(n.d.). Retrieved from http://psycnet.apa.org/record/2009-10620-001
(n.d.). Retrieved from https://www.uptodate.com/contents/acute-treatment-of-migraine-in-adults
(n.d.). Retrieved from http://www.medlink.com/article/status_migrainosus
Basic Principles. (2013, May 06). Retrieved from http://gonstead.com/gonstead-system/basic-principles/
Chaibi, A., & Tuchin, P. J. (2011, September). Chiropractic spinal manipulative treatment of migraine headache of 40-year duration using Gonstead method: A case study. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3259914/
Dunleavy, B. P., & Chua, J. P. (2021, March 2). Nerve Stimulation Devices for Migraine Treatment | Everyday Health. EverydayHealth.Com. https://www.everydayhealth.com/migraine/guide/treatment/nerve-stimulation-devices/
Gallagher, R. M., & Mueller, L. (2003, 10). Managing Intractable Migraine With Naratriptan. Headache: The Journal of Head and Face Pain, 43(9), 991-993. doi:10.1046/j.1526-4610.2003.03191.x
Howard, J. (2016, October 20). How your mouth is linked to your migraines. Retrieved from https://www.cnn.com/2016/10/20/health/migraine-triggers-bacteria/index.html
Ketamine Shows Promise in Easing Intractable Migraine Pain. (2017, October 23). Retrieved from https://psychcentral.com/news/2017/10/23/ketamine-shows-promise-in-easing-intractable-migraine-pain/127814.html
Krusz, J. C., Scott, V., & Belanger, J. (2000, March). Intravenous propofol: Unique effectiveness in treating intractable migraine. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/10759925
Kurth, T., Schurks, M., Logroscino, G., & Buring, J. E. (2009). Migraine frequency and risk of cardiovascular disease in women. Neurology, 73(8), 581–588. https://doi.org/10.1212/wnl.0b013e3181ab2c20
Meritas Health. (n.d.). New Nerve Block Procedure Effectively Treats Migraines. Retrieved June 16, 2021, from https://www.nkch.org/for-providers/newsletter/physician-connections-articles/past-issues/2016/july-august/new-nerve-block-procedure-effectively-treats-migraines
Migraine.com. (2012, January 9). What is Status Migrainosus? https://migraine.com/blog/what-is-status-migrainosus
NICE (National Institute for Health and Care Excellence). (2013, April). Treating intractable chronic migraine by stimulating nerves at the back of the head. https://www.nice.org.uk/guidance/ipg452/resources/treating-intractable-chronic-migraine-by-stimulating-nerves-at-the-back-of-the-head-pdf-364807117
NOAA Office of Response and Restoration, US GOV. (n.d.). Search Chemicals. Retrieved from https://cameochemicals.noaa.gov/reactivity/documentation/RG69-RG69
New Nerve Block Procedure Effectively Treats Migraines. (n.d.). Retrieved from http://www.nkch.org/physicians/newsletter/past-issues/2016/julyaug-2016/new-nerve-block-procedure-effectively-treats-migraines/
Optics, A. (2018, January 17). Cold Weather Migraines: How to Prevent Winter Migraines. Retrieved from http://www.axonoptics.com/2018/01/preventing-cold-weather-migraines/
Optics, A. (2017, April 28). How Well Do You Know Your Migraine Triggers? Retrieved from http://www.axonoptics.com/2016/06/well-know-migraine-triggers/
Optics, A. (2017, December 27). Natural Migraine Remedies: A Comprehensive Guide. Retrieved from http://www.axonoptics.com/2017/11/natural-migraine-remedies/
Optics, A. (2017, March 15). Reviewed: Top 5 Migraine Tracking Apps. Retrieved from http://www.axonoptics.com/2017/02/top-5-migraine-tracking-apps/
Optics, A. (2017, November 17). What Migraine Medications are Available to Me? Retrieved from http://www.axonoptics.com/2017/08/migraine_medications_available/
Rankin, L. (2011, March 31). 11 Natural Treatments For Depression: An MD’s Tips For Skipping The Prozac. Retrieved from https://www.psychologytoday.com/blog/owning-pink/201103/11-natural-treatments-depression-md-s-tips-skipping-the-prozac
Schwenk, E. S., Dayan, A. C., Rangavajjula, A., Torjman, M. C., Hernandez, M. G., Lauritsen, C. G., ... & Viscusi, E. R. (2018). Ketamine for refractory headache: a retrospective analysis. Regional Anesthesia & Pain Medicine, 43(8), 875-879.
Seng, E. K., Buse, D. C., Klepper, J. E., J. Mayson, S., Grinberg, A. S., Grosberg, B. M., Pavlovic, J. M., Robbins, M. S., Vollbracht, S. E., & Lipton, R. B. (2017). Psychological Factors Associated With Chronic Migraine and Severe Migraine-Related Disability: An Observational Study in a Tertiary Headache Center. Headache: The Journal of Head and Face Pain, 57(4), 593–604. https://doi.org/10.1111/head.13021
Spierings, E. L. (2014, January 08). Daily Triptan Use for Intractable Migraine. Retrieved from http://onlinelibrary.wiley.com/doi/10.1111/head.12275/abstract
Tewfik, T. L. (2017, November 28). Trigeminal Nerve Anatomy: Gross Anatomy, Branches of the Trigeminal Nerve, Microscopic Anatomy. Medscape. https://emedicine.medscape.com/article/1873373-overview
Tso, A. R., & Goadsby, P. J. (2017). Anti-CGRP Monoclonal Antibodies: the Next Era of Migraine Prevention? Current Treatment Options in Neurology, 19(8). https://doi.org/10.1007/s11940-017-0463-4
US9606277B2 – Apparatus and methods for reducing frequency or severity of photophobic responses or modulating circadian cycles. (n.d.). Retrieved from https://patents.google.com/patent/US9606277B2/en
Zhu, S., & Trinh, V. T. (2021, May 6). Status migrainosus. MedLink Neurology. https://www.medlink.com/articles/status-migrainosus