The word “phobia” typically is associated with feelings of anxiety or fear, but not every type of phobia elicits such fearful emotions.
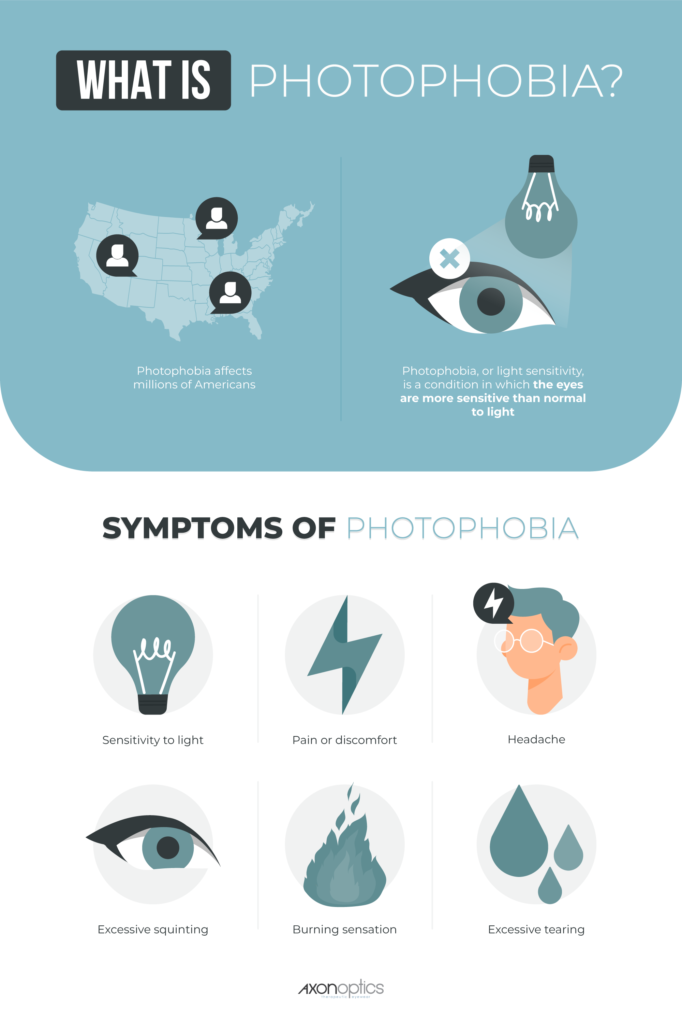
Photophobia, or light sensitivity, is a condition associated with extreme sensitivity to lights. It can cause reactions like squinting, continual blinking, excessive tearing and even headache and nausea.
Jen, a customer of ours, wrote, "As a young child I was called a bat because I couldn’t handle light and was much happier in the dark or dusk." She tried to control the intermittent, unpredictable light sensitivity pain by using "sunglasses, computer glasses, you name it".
In the following infographic and guide we draw insights from academic studies to better understand the diagnosis, symptoms, and treatment of photophobia.
Contents
- Photophobia symptoms
- What causes photophobia?
- How is photophobia diagnosed?
- How does photophobia cause pain?
- How is photophobia treated?
- Photophobia prevention at home
- What NOT to do for photophobia
- Light-filtering lenses
- Takeaways
- FAQs About Light Sensitivity
- References
Photophobia symptoms
Each individual is unique and is likely to experience symptoms differently based on the underlying cause. Photophobia symptoms may include:
- Sensitivity to light
- Pain or discomfort
- Headache
- Nausea
- Excessive squinting or blinking
- Burning sensation
- Excessive tearing
What causes photophobia?
Most people with photophobia have an underlying condition. Migraine, chronic headaches, chronic dry eye, blepharospasm (involuntary closing of the eyelids) and brain injuries are conditions associated with photophobia.1
For example, research has shown patients with migraines are more sensitive to light, and those who suffer from migraines and some other types of chronic headaches tend to have a lower tolerance of bright light. 2,3 The following are the most common conditions causing photophobia:

Other potential causes of photophobia include:

How is photophobia diagnosed?
It's relatively rare for a patient to visit an eye doctor “simply” as a result of light sensitivity; instead, photophobic symptoms are usually revealed during an exam scheduled for another issue, such as eye discomfort, blurry vision, migraine, or migraine aura (sometimes called ocular migraine).
During the exam it's important to mention any issues with light sensitivity, including sensitivity that occurs only in the presence of certain types of light such as fluorescent lights since these lights are more likely to induce photophobic symptoms.
Many photophobic patients have fewer symptoms in natural light compared to indoor lighting, a difference that can aid in making a diagnosis of photophobia.

How does photophobia cause pain?
A Vision Pathway and a Pain Pathway: Thinking back to grade school, we learned that images are formed when light enters through the pupil and refracts through the lens which focuses the light on the retina. Signals pass from the retina along the optical nerve to the brain where an image is processed!

Light is transmitted through your eyes to your brain, but what you probably didn't know is that there is a SEPARATE pathway from your eye to the brain that transmits pain - or rather makes us sensitive to light.
Why would we need to be light sensitive? It actually prevents people from staring at bright lights that could damage the very sensitive photoreceptor cells that line the eye's retina. For example, looking at the sun is painful and causes people to look away.
This particular light sensitive reaction is a good thing because excessive sunlight would damage the eyes.
So how exactly, does the light cause pain? Until recently, it was not clear how bright light could be turned into painful sensations and reactions like blinking and squinting. For years researchers hypothesized there was a sort of “transducer” in the eye that converted light into pain. 4
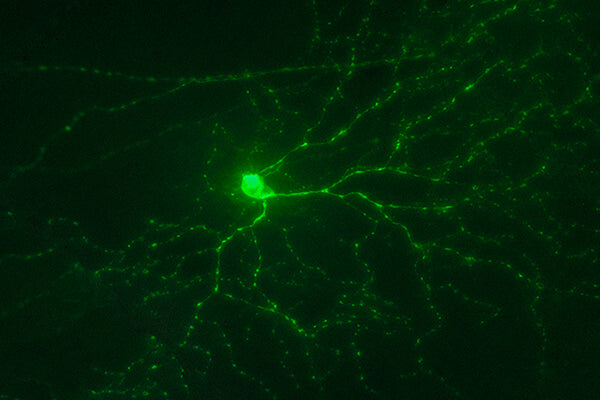
Advances in technology and techniques have enabled researchers to finally confirm that a transducer exists. They are unique light sensitive cells in the back of the eye called -- get ready for this -- intrinsically photosensitive retinal ganglion cells (ipRGCs or melanopsin cells).
The discovery of these cells is one of the most important advances in understanding photophobia!
Animal studies show that this is where the pain pathway starts and that these cells send signals to the pain centers in the brain.5 It's this cell-to-brain connection that researchers believe may play an integral role in photophobia and its symptoms.

IPRGC cells or melanopsin cells transduce light into pain.
Image Credit: GFP positive ganglion cell provided by Ning Tian, M.D., Ph.D., photographed by Bryan William Jones, Ph.D.
Hypersensitivity: Everyone has sensitivity to light as described above, however, some people are “hypersensitized” and have discomfort in normal lighting conditions that are otherwise comfortable for most people.6
Those with hypersensitive ipRGC cells may experience discomfort in locations with harsh fluorescent lighting such as big box stores, schools, and offices or from car headlights and sunlight reflecting off of water.
Amazingly, studies have shown that light can trigger pain even in blind patients because the pain pathway is separate from the vision pathway.
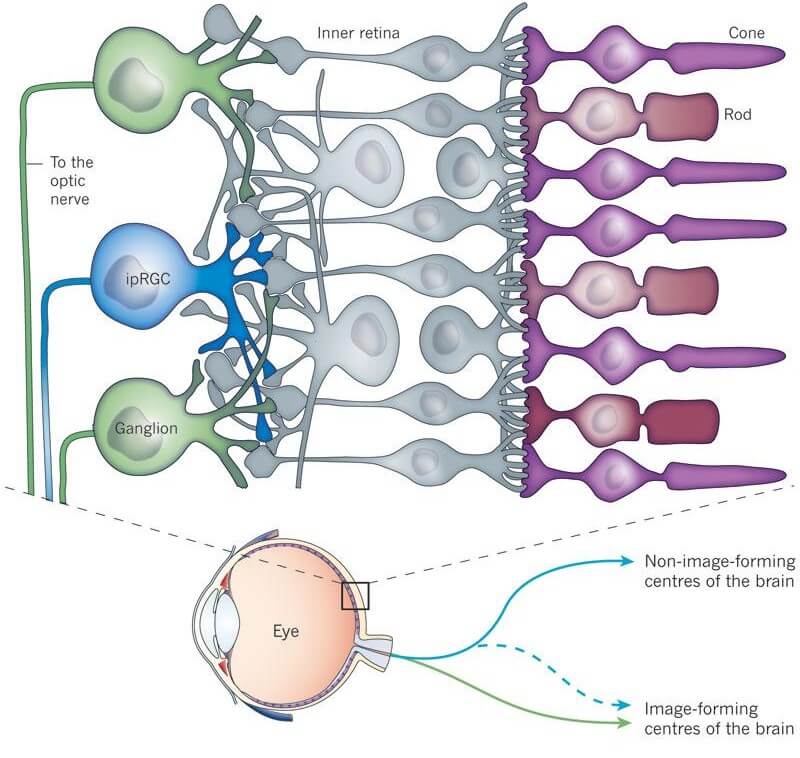
Image Credit: Published online 19 January 2011 | Nature 469, 284-285 (2011) | doi:10.1038/469284a
Importantly, the ipRGCs cells that form the beginning of the pain pathway are most reactive only to certain wavelengths of light (the blue and amber portion of the light spectrum). That means that only a small portion of the light you see aggravates hypersensitivity. This sensitivity to blue and amber light plays a key role in treatment which is discussed below. The deep stuff: This gets into the nitty gritty details of the pain pathway. If you'd like, just skip to the 'how is photophobia treated?' section. Three possible pain pathways have been identified:
1. The first pathway involves the trigeminal nerve, a major nerve with multiple branches, one of which is the ophthalmic branch. In this pathway, light reaching the ophthalmic branch activates the main trigeminal nerve causing blood vessels to dilate and stimulating pain-sensitive neurons in the blood vessels.
2. In the second pathway, a “direct route” connects the IPRGCs with the thalamus, the brain's pain center, using the optic nerve as its conduit.
3. The third pathway involves special transducers that can stimulate the trigeminal nerve in other ways, causing photophobic symptoms even if the optic nerve has been damaged or destroyed. These transducers may be the IPRGCs or there may be other melanopsin-containing cells acting on the nerve.
Scientists say these three pathways interact in different ways and that more pathways may exist that have yet to be discovered.
How is photophobia treated?
The first step in treating photophobia is to have a comprehensive eye exam to rule out other possible causes of light sensitivity, and also to reveal other conditions that commonly occur along with photophobia, like dry eye syndrome, and blepharospasm.

Understanding all the contributing factors is an important part of diagnosis and treatment since the underlying or contributing causes can have a significant bearing on the type of therapy selected.
For instance, patients with dry eye syndrome will receive care for those symptoms to determine if their photophobic symptoms resolve, partially or completely, once the eyes are properly and regularly lubricated.
Treatment for dry eyes can include special lubricating eye drops (either over-the-counter or prescription), topical or oral medications, and minor procedures to help restore tear production and flow. Patients who have photophobic symptoms associated with migraines or blepahrospasm may benefit from other treatments, which can include oral medications, BOTOX® injections and other therapies.
Photophobia prevention at home
Once the underlying cause has been determined, a few practical tips can help minimize photophobia.- Use polarized sunglasses when outdoors
- Wear a hat or cap when outdoors
- Avoid bright fluorescent lights
- Utilize natural light where possible for indoor settings
- Control indoor lighting with dimmers and consider replacing any fluorescent or cool white LED light bulbs with a warm white LED light bulb or an incandescent light bulb.
- Control the brightness on your screen by adjusting the settings on your TV, computer, phone and other devices
- Wear light-filtering lenses or tinted lenses indoors
At home is where we have the greatest ability to control our light environment.
One of the biggest challenges is how to prevent photophobia in the workplace, supermarket, shopping centers which often use bright and cheap lighting. Even driving at night with other car headlights can very uncomfortable.
What NOT to do:

Wearing sunglasses indoors can make your condition worse and is strongly discouraged. 1
Sunglasses inside might provide relief initially, but it is likely to make your light sensitivity worse over time. By wearing dark glasses indoors, you are dark-adapting your retina which aggravates sensitivity to light. 1
We see this dark adaption occurring all the time. For instance, when we come out of the movie cinema in the middle of the day and face the bright sunlight it causes discomfort (even for people without light sensitivity). This is because their eyes have adapted to the dark cinema theater for the last 2 hours.
Wearing sunglasses inside has a similar affect which can worsen our photophobia.
Instead, use lenses that are specifically intended for indoor use. Use of these lenses inside will not result in dark adaption of the retina.
Light-Filtering Lenses
Specially-tinted lenses are designed to block wavelengths most commonly associated with triggering photophobia symptoms without blocking other types of light so vision remains clear and unimpeded.
No matter what the underlying cause, patients with photophobia may benefit from the use of specifically designed tinted lenses.8

Sometimes called FL-41 lenses, these lenses reduce exposure to the wavelengths most likely to cause photophobia reactions. 1
Light-filtering lenses can provide patients with a simple method of reducing the likelihood of migraines and other light-mediated symptoms.
These lenses ensure you get the light-filtering technology you need without impairing vision or causing other issues like blurry vision, eye strain or headaches.
Takeaways
- Photophobia affects millions of people.
- Photophobia is closely linked with migraines, and researchers believe light-sensitivity can lead to the development of migraine symptoms.
- Light sensitivity involves a complex series of events promulgated by special cells called intrinsically photosensitive retinal ganglion cells (ipRGCs).
- Photophobia symptoms can exist even when we don't “see” light.
- Some symptoms may resolve with treatment of an underlying condition such as dry eye syndrome.
- People with photophobia can be helped by wearing light-filtering lenses to block out the wavelengths most likely to cause symptoms.
FAQs About Light Sensitivity
– Answered by Dr. Katz, MD, PhD, of the Moran Eye Institute at the University of Utah Medical Center
Q: What is light sensitivity?
A: Everybody has a little light sensitivity. If you look at a light that’s too bright, like the Sun, it hurts, and that’s a protective mechanism that we all share. But in some people, such as people who suffer from blepharospasm or migraines, their sensitivity to light is amped up, so that even normal amounts of light that shouldn’t bother people become noxious and painful.
Q: Why do migraines cause light sensitivity?
A: We don’t really know why migraines cause light sensitivity, but it’s clear nearly everyone with migraine will tell you that they have sensitivity to light during an attack and many patients with migraine will tell you that certain kinds of light can trigger an attack (particularly those found in big box stores such as Target and Walmart).
A certain number of people are chronically light sensitive, even when they don’t have a migraine. But the physiology behind why people are light sensitive is just now barely being understood.
Q: Is there treatment for light sensitivity?
A: We really don’t have any pharmacologic treatment for sensitivity to light. What we do have are optical treatments, or natural treatments to light sensitivity. So there are ways that we can reduce the amount of light coming into your eye that’s going to be painful and make you more comfortable.
For those sensitive to sunlight you should put on a pair of sunglasses, but to reduce your sensitivity to light indoors and still be able to do your job and to function, sunglasses just don’t work. And that’s why we Axon Optics is powered by Avulux Migraine & Light Sensitivity Lenses to help manage the impact of light on people's lives, make people more comfortable, and allow them to continue to work indoors.
Axon now offers a wide range of styles for light sensitivity glasses designed for either indoor or outdoor use.

Q: If I don’t like to wear sunglasses, what can I do about my sensitivity to light?
A: The best method, if possible, is to manage the underlying cause of your light sensitivity and to use tools like sunglasses outdoors or tinted glasses indoors/outdoors to reduce the impact of light on your life.
Q: Are there certain types of syndromes that make people more susceptible?
A: At this time we’re not aware of any syndromes that would predispose somebody to light sensitivity. However, the big conditions that are usually associated with light sensitivity are migraine, blephoraspasm, and traumatic brain injury. Those three conditions account for probably 99% of the light sensitive patients that I see in my clinic.
Q: What’s the difference between using Botox and tinted glasses for light sensitive migraines?
A: These therapies can be complementary. They’re addressing two different things. With Botox injections, you’re trying to reduce the sensitivity around the face and to decrease the frequency and severity of headaches. With tinted glasses, you’re trying to decrease the amount of light coming in that’s irritating the eyes and generating a migraine, making people more uncomfortable. So it’s not really an either/or, it’s a complementary approach. They work by different mechanisms and they can work together.
Q: Why can eyes be sensitive to light?
A: All of our eyes have light sensors in them that keep us from looking at a light that’s too bright and can damage our eyes. It’s a protective mechanism and probably helped you when you were a child to not stare into the sun which would damage your eyesight.
However, in some people that protective mechanism is simply too sensitive and I believe that’s what leads to photophobia (light sensitivity) and conditions such as migraine and blephoraspasm.
Q: Are people with light-colored eyes more sensitive than those with darker colored eyes?
A: The notion that people with light colored or blue eyes are more light sensitive than people with brown colored eyes is simply not true.
There are people that have a condition called albinism and they don’t have the normal pigment in their skin or in their eyes. Those people are profoundly light sensitive and they universally have blue eyes, so that might be part of the misconception.
References
This article is based on research from Drs. Kathleen Digre and Bradley Katz and their publication "Diagnosis, pathophysiology, and treatment of photophobia" from the Journal Survey of Ophthalmology and research from Drs. Digre and KC Brennans publication "Shedding Light on Photophobia" from the Journal of Neuroophthalmology. These researchers are in the Department of Ophthalmology and Neurology at the University of Utah.